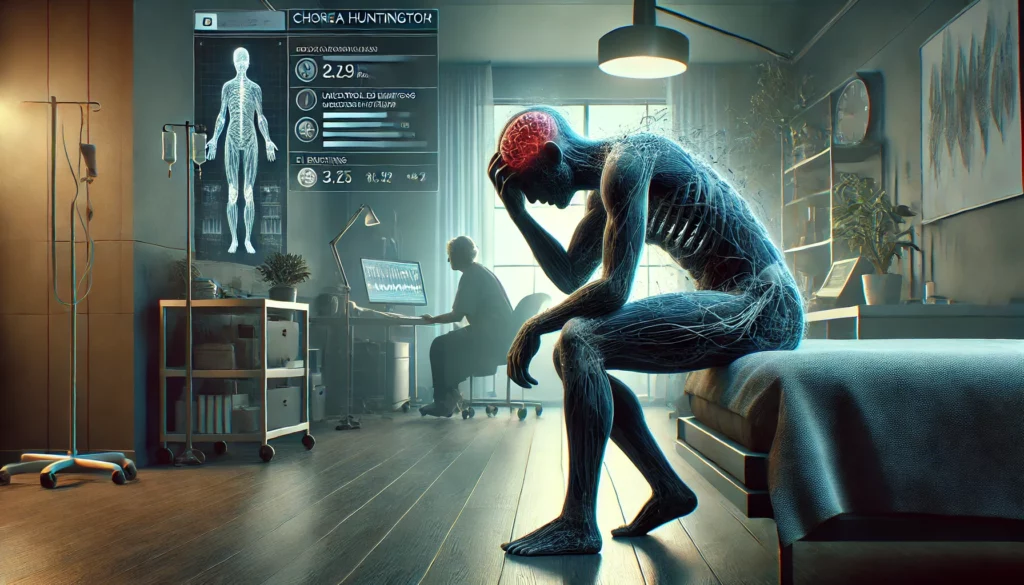
Chorea Huntington (CH) is a genetically determined neurodegenerative disease that affects both the motor nervous system and mental health. Psychological changes often appear years before the characteristic motor symptoms, including mood swings, behavioral issues, and cognitive impairments. Studies suggest that patients with Huntington’s disease frequently exhibit symptoms resembling bipolar or unipolar disorders.
But how exactly are Huntington’s disease, bipolar disorder, and depression related? Are there similarities, or are they fundamentally different conditions?
🧠 1. What Is Chorea Huntington?
Huntington’s disease is an autosomal dominant inherited disorder, caused by a mutation in the HTT gene on chromosome 4. This mutation leads to an abnormal accumulation of the huntington protein, damaging neurons in the striatum (basal ganglia) and other brain regions.
🔹 Key Characteristics of Huntington’s Disease:
✔ Involuntary, jerky movements (chorea)
✔ Cognitive impairments & progression to dementia
✔ Psychiatric symptoms such as depression, irritability & impulsivity
📌 Psychiatric symptoms often appear years before the first motor impairments!
🔄 2. Psychiatric Symptoms of Huntington’s Disease Compared to Bipolar & Unipolar Disorder
Huntington’s disease is not primarily a psychiatric disorder, but it shares many similarities with affective disorders, especially bipolar disorder and unipolar depression.
| Feature | Huntington’s Disease | Bipolar Disorder | Unipolar Depression |
|---|---|---|---|
| Cause | Genetic (HTT mutation) | Multifactorial (genetic & environmental) | Multifactorial (biological, psychological & social factors) |
| Mood Instability | Frequent, uncontrolled, irritability | Alternating between mania & depression | Persistent low mood |
| Impulsivity & Disinhibition | Very common, uncontrolled | Common in mania | Rare |
| Cognitive Deficits | Strongly pronounced, progressively worsening | Possible cognitive impairments in severe episodes | Common concentration issues |
| Suicide Risk | High, especially in early stages | Increased, especially during depression | Increased |
| Course | Progressive, worsening over time | Episodic, with possible relapses | Episodic or chronic |
| Treatment | Symptomatic treatment, no cure | Mood stabilizers & psychotherapy | Antidepressants & psychotherapy |
📌 While bipolar and unipolar disorders primarily involve neurotransmitter dysregulation, Huntington’s disease is a progressive neurological disorder with psychiatric symptoms.
🔬 3. Why Do Bipolar & Depressive Symptoms Occur in Huntington’s Disease?
🔹 Brain Changes
The primary affected regions in CH are the basal ganglia and striatum, which are deeply involved in mood regulation and impulse control.
- Degeneration of basal ganglia → Disrupts dopamine and serotonin systems
- Neurotransmitter imbalance → Patterns similar to those in bipolar disorder
- Cognitive decline & emotional instability → Worsens depression & irritability
📌 The damage to these brain areas explains why Huntington’s disease has such strong psychiatric effects.
💊 4. Treatment Approaches: Similarities & Differences
🔹 Therapeutic Strategies for Huntington’s Disease vs. Bipolar & Unipolar Disorders
| Treatment | Huntington’s Disease | Bipolar Disorder | Unipolar Depression |
|---|---|---|---|
| Medication | Antipsychotics, tetrabenazine, antidepressants | Mood stabilizers (lithium, valproate), antipsychotics | SSRIs, SNRIs, atypical antidepressants |
| Psychotherapy | Supportive, cognitive behavioral therapy | Cognitive behavioral therapy, psychoeducation | Cognitive behavioral therapy, psychodynamic therapy |
| Neuroprotective Measures | Exercise therapy, nutrition, symptom management | No specific neuroprotection | No specific neuroprotection |
📌 While bipolar & unipolar disorders can be stabilized with psychotherapy & medication, there is no curative treatment for Huntington’s disease – only symptomatic management.
🎯 5. Conclusion: How Are Huntington’s Disease, Bipolar & Unipolar Disorder Connected?
✔ Huntington’s disease can trigger psychiatric symptoms resembling bipolar or unipolar disorders.
✔ Depression is highly common in CH patients, increasing suicide risk.
✔ Manic or impulsive behaviors in CH can be mistaken for bipolar disorder.
✔ Neurobiological overlaps exist in the dysregulation of dopamine & serotonin.
✔ Treatment differs: While bipolar/unipolar disorders are stabilizable, CH remains progressive.